Dr. McBride is a Professor at the Texas Tech University Health Sciences Center School of Nursing whose research focus is on methods development for implementing, evaluating and utilizing health information technology to address patient safety, quality and population health. Dr. McBride was the Principal Investigator for a Texas Statewide Study of Nurses Satisfaction with their electronic health records. She is a professor with teaching responsibilities supporting graduate courses in statistics, informatics, and epidemiology. She is a Fellow in the Academy of Nursing and sits on the Information Technology and Informatics Expert Panel.
Mari Tietze, PhD, RN-BC, FHIMSSDr. Tietze is a Professor at the Texas Woman's University (TWU) College of Nursing, teaching informatics courses focused on interprofessional collaborative practice and Director of the Graduate Certificate in Interprofessional Informatics program. Dr. Tietze is the Doswell Endowed Chair for Nursing Informatics aimed at advancing nursing informatics at TWU. Since 2010, she has been the co-chair of the Texas Nurses Association/Texas Organization of Nurse Executives Health Information Technology committee to represent nurses' experiences related to information technology use in their practice of patient care delivery. Research focus is telehealth with a telemedicine, remote management and mobile health component. Dr. Tietze has been certified since 2000 by ANA in Informatics Nursing.
Catherine Robichaux, PhD, RN, APRN, Alumna CCRNDr. Robichaux is an Adjunct Assistant Professor at University of Texas Health; San Antonio, Texas and The University of Mary in Bismarck, North Dakota. She has taught ethics at the undergraduate and graduate levels and conducted research on moral distress and ethical climate among other issues. Catherine was a member of the Steering Committee to revise the Code of Ethics and is currently a member of the ANA Ethics Advisory Board.
Liz Stokes, JD, MA, RNMs. Stokes is the Director of the American Nurses Association Center for Ethics and Human Rights. She worked for several years as a critical care nurse and later received her law degree. She worked as a consultant for the D.C. Board of Nursing interpreting professional ethics provisions and recently completed her masters in bioethics. Her leadership is demonstrated through various charitable roles. Liz serves as an Associate Editor for the Journal of Bioethical Inquiry and is a volunteer with the D.C. Bar Association. She is currently an American Academy of Nursing Jonas Health Policy Scholar.
Eileen Weber, DNP, JD, BSN, PHN, RNDr. Weber is a nurse attorney and Clinical Assistant Professor at the University of Minnesota School of Nursing, where she teaches ethics, leadership, and public policy in the context of a continuum of interprofessional healthcare. She founded and leads the Upper Midwest Healthcare Legal Partnership Learning Collaborative. She serves on the American Nurses Association Center for Ethics and Human Rights Advisory Board and the University of Minnesota Medical Center (Fairview) ethics committee.
With the passage of the Health Information Technology for Economic and Clinical Health Act in 2009, the United States, as of 2017, has achieved 95% saturation with electronic health records as a means to document healthcare delivery in acute care hospitals and guide clinical decision making. Evidence is mounting that EHRs are resulting in unintended consequences with patient safety implications. Clinical teams confront usability challenges that can present ethical issues requiring ethical decision-making models to support clinicians in appropriate action on behalf of safe, effective clinical care. The purpose of this article is to identify and address ethical issues raised by nurses in use of electronic health records. We provide a case scenario with application of the Four Component Model and describe a study of nurse experiences with the EHR. The nursing Code of Ethics, Nursing Scope and Standards, and Legal Implications are reviewed, and we conclude with recommendations and a call to action.
Key Words: electronic health records, ethics, ethical decision making, moral distress, usability, unintended consequences, patient safety, quality, Health Information Technology, Rest Four Component Model
Healthcare delivery in the United States (U.S.) is changing at a rapid pace to keep up with the ever-growing population health needs and for management of chronic diseases (Healthy Aging Team, 2017). With the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009 (U.S. Department of Health and Human Services, 2012), the United States, as of 2017, has achieved a 95% saturation with electronic health records (EHRs) as a means to document healthcare delivery in acute care hospitals and guide healthcare delivery clinical decision making (Office of National Coordinator for Health Information Technology, 2017). Approximately 60% of U.S. office-based physicians have an EHR implemented and in use.
. in many respects, care has improved with use of technologies. Collectively, these trends impact nurses nationwide across all care settings. Studies have indicated that, in many respects, care has improved with use of technologies and, when meaningful use of EHRs is fully achieved and experienced by nurses, they are much more likely to be satisfied with the EHR (McBride, Tietze, Hanley, & Thomas, 2017). Evidence is mounting that these same systems are also resulting in unintended consequences with patient safety implications, potentially contributing to provider moral distress (Henry, Pylypchuk, Searcy, & Patel, 2016). Clinical teams often confront usability challenges that present ethical issues and require ethical decision-making models to support clinicians with appropriate action on behalf of safe and effective clinical care.
Clinical teams often confront usability challenges that present ethical issues. The purpose of this article is to identify and address ethical issues raised by nurses in use of EHRs. We provide a case scenario with application of the Four Component Model (FCM) (Rest, 1986). To do this, a clinical case study will be presented, along with discussion of nurse experiences using the EHRs in a recent study (McBride, Tietze, Hanley, & Thomas, 2015). Then, recommendations and a call to action are made based on the FCM in light of nursing practice standards, ethical issues, and where applicable legal issues.
. formulaic alerts can present challenges to clinical decision making. One strength associated with certified EHRs under the HITECH Act of 2009 for supporting patient safety and quality is that evidenced-based protocols can be reinforced by using clinical decision support (CDS). CDS is designed to trigger, or alert, the clinical team with the right information, through the right channels, to the right person, at the right time, for the right patient, via the correct route of the EHR or supporting technologies (Osheroff et al., 2012). These same formulaic alerts can present challenges to clinical decision making for clinical teams working with an actual patient, raising practical and ethical considerations.
When examining ethical issues and applying frameworks to analyze a situation, clinical scenarios often help to ground discussions of problems in the day-to-day clinical care that commonly occur in healthcare delivery. The following case presents a scenario for applying a framework to address ethical concerns that nurses have raised regarding the function of some EHRs.
She suspects that the afebrile patient does not have sepsis, but instead has an exacerbation of HF with possible pulmonary edema. Nancy has worked in a busy community hospital emergency department (ED) for over ten years. She is caring for a patient that presents to the ED with the following:
These symptoms trigger the EHR CDS alert for sepsis because the patient scored high on the hospital sepsis screening tool built within the EHR. The CDS fires alerts that prompt the ordering physician to fluid resuscitate the patient according to the Center for Disease Control guidelines for suspected sepsis. Nancy recognizes that not only does this patient have symptoms that could be evolving sepsis, but the EHR indicates the patient has previously been admitted for fluid overload from heart failure (HF). She suspects that the afebrile patient does not have sepsis, but instead has an exacerbation of HF with possible pulmonary edema because the patient also exhibits 2+ pitting edema and crackles in both lung bases.
The ED physician follows the CDS sepsis alerts that call for fluid resuscitation. The ED physician follows the CDS sepsis alerts that call for fluid resuscitation. Nancy questions the doctor order for aggressive fluid bolus and relates her concern that the patient is not septic. She points out the history of HF, which creates a risk for fluid overload with the bolus. The physician agrees with the nurse but states, "just drip it in slow, otherwise if we don’t follow protocol we may fall out of the sepsis quality metric for the hospital. I don’t want to send this patient to the ICU and have it later determined to be a sepsis case that we didn’t follow protocol on!"
[Nancy] feels very distressed but hopes for the best outcome for this patient. No order for a slow drip was noted in the EHR, with only a verbal instruction on a busy ED shift for a patient ready for transfer to the ICU. Nancy questions the appropriateness of the physician orders, but follows physician instructions. She feels very distressed but hopes for the best outcome for this patient. She subsequently reports the request by the physician to drip slowly in a verbal handoff to the ICU nurse who receives the patient. The ICU nurse, recognizing that the drip does not follow the EHR recorded order, opens up the drip according to the computer provider order entry (CPOE). The patient has respiratory arrest. The patient requires intubation due to flash pulmonary edema with a subsequent diagnosis of acute onset of exacerbated fluid overload, secondary to rapid administration of intravenous (IV) fluid bolus and complication of HF. The attending intensivist on duty determines that the patient does not have sepsis.
This case presents a scenario happening across the nation in terms of EHR triggered protocols that capture electronic quality measures, often tied to value-based purchasing payer models upon which the organization will be penalized in the event measures are not met. This case study illustrates evolving guidelines that require clinical teams to use critical thinking skills when presented with CDS or information within the EHR that is not aligned with the clinical judgment of the entire clinical team. Further, this case offers several ethical considerations for examination. The scenario also reinforces nurses’ statements as reported in 2015 via the Texas Nurses Association-Texas Organization of Nurse Executives (TNA-TONE) statewide study on EHRs (McBride et al., 2015). For example, the following was one of 352 statements by nurses about EHR experiences:
Yes, the documentation of "quality standards" has greatly improved, but patient care and patient safety has not. In fact nurses have to enter false information sometimes and work around the system (I use vendor X, Y and Z) and all have similar issues. I know first-hand of 2 sentinel events caused by the systems (X and Y). Also systems audits are being used to evaluate and discipline nurses; this is a big ethical issue as nurses are charting stuff for the wrong reasons/. creating a conflict of interest.
This case scenario can be examined in terms of the overall context of ethical implications in use of the EHR. We can also consider the distress that can occur when protocols/guidelines; clinical decision support systems; nurse-patient relationship; and clinical communications between and among teams conflict with a nurse's code of ethics.
As a result of the HITECH Act in 2009, the TNA Board of Directors formed a Health Information Technology advisory committee. This committee was to evaluate the changing health technology environment and make recommendations to the TNA Board regarding steps needed to prepare Texas nurses for the rapid uptake of technology in healthcare settings required by this legislation. The TNA Board joined with the Texas Organization of Nurse Executives (TONE) to create a statewide partnership with nursing leaders to address the impact of health information technology (HIT) on nursing in the state of Texas.
The TNA-TONE HIT committee was charged with examining how Texas nurses were impacted by newly implemented EHRs across the state and to establish baseline measures of nurse satisfaction to inform evidence-based improvement strategies. A statewide study was initiated to evaluate nurse perceptions about clinical information systems such as EHRs.
. analysis of text comments found patterns and trends that reflected distress related to moral issues and ethical dilemmas. Quantitative results from the statewide study indicated that nurses were 84% more likely to be satisfied when they reported high scores related to a meaningful use maturity sensitivity index (MUMSI). The MUMSI allowed for analysis that addressed differing levels of functional status, or maturity of the given EHR using the meaningful use (MU) measures as a proxy for maturity (McBride et al., 2017). However, analysis of text comments found patterns and trends that reflected distress related to moral issues and ethical dilemmas (please note that we are using the terms "moral" and "ethical" interchangeably in accordance with the current literature). We believe the ethical issues, in particular, warrant further exploration and require models of decision making to support clinical interprofessional teams in appropriate decision-making and subsequent action.
In the Texas-based statewide study (McBride et al., 2015), researchers elicited additional information to learn about experiences of nurses using EHRs with this open-ended statement: “We are interested in your feedback and anything we might not have covered, please provide any additional information you care to provide.” Just over 30% (352 of 1,157 participants) provided written comments about their experiences.
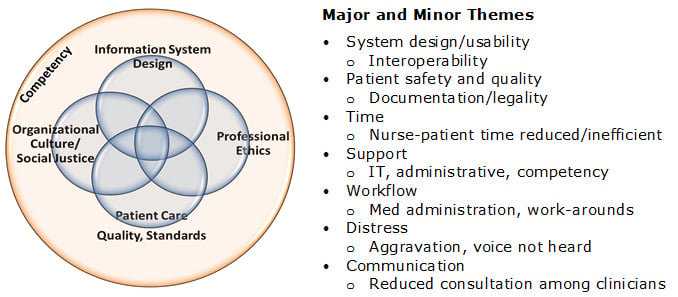
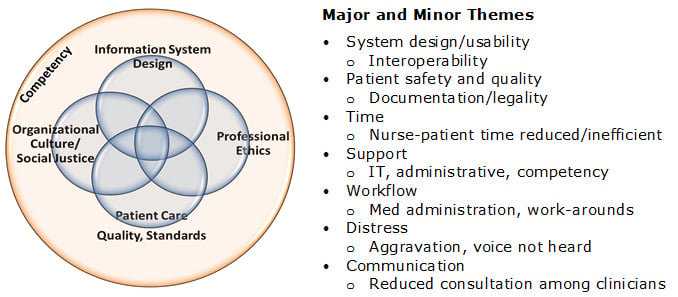
A thematic content analysis of the narrative responses to the open text question was used to analyze the data. Texts were organized in a spreadsheet and reviewed systematically by two qualitative researchers from the TNA/TONE committee research subgroup to identify key concepts. The text narrative responses were then reorganized according to concepts and summarized into categorical statements. Further immersion and analysis of the categories by two researchers with informatics expertise resulted in a synthesis of comments within the categories that revealed several primary themes. These are noted in Figure 1.
A conceptual model that reflects the overall common concepts detected in the thematic analysis was developed by the research group and is also noted in Figure 1. Note that “Patient Safety and Quality” is a major theme, with a minor theme “documentation/legality.” This suggested that practice challenges associated with patient safety and quality were experienced. We learned that these were reflected, among other ways, in the EHR-based documentation that varied from established interprofessional practice standards. Although the case study and the Texas nurses’ comments reflected ethical issues raised by nurses, there are significant implications for the entire care team given the EHR is the primary means of interprofessional communication.
Figure 1. Major and minor themes related to qualitative study comments.
A sampling of these comments is provided by categories in Table 1. They are grouped by category of content.
Table 1. Comments by Nurses about their EHR Experience
Category
Comment
Training
I have almost no training on the "System.” I have to fumble around to do anything on this "System" and it is purely an accident when I do find what I need.
Documentation
System was not designed by the people who would use it. It does not capture the data required by the state to successfully use it. We are unable to see any notes/assessments that we did not personally input. Very frustrating because we constantly have to do double work.
Sometimes the canned responses to questions do not have the appropriate answer listed as an option, and the only way to complete the documentation is to go to another menu and enter a nurse’s note. Our preop department uses entries in both the nursing module and the OR module, which necessitates constantly switching from one menu to another - time consuming and inefficient.
The "copy/paste" function has made it easier for providers to not write new original assessments. Because most of the notes are copy and pasted, there are many discrepancies (on one line, the patient is intubated; on the next line of the same patient, the patient is on nasal cannula). It's made the notes semi-worthless.
This system has quadrupled our workload. It is not accurate and orders tend to disappear. The pharmacy part allows expired orders to carry on and continue to be active even after stop dates which lead to medication errors. This system is difficult to view orders and communicate with others. Things do not work well. It takes several hours to get thru discharges due to links that do not work. With the ER after two weeks on the program, it developed an application error that would not let nurses go back to add information while the patient is still active and document is active.
Equipment
Our computers at times freeze inside the room. During am med pass, it is so stressful finding a good computer that does not freeze. Sometimes I have to go through 3-5 computers before finding one that works.
Critical Thinking
Sometimes I feel that the barcode scanning system for medication administration hinders critical thinking and prevents truly looking at what you are giving the patient.
The FCM describes the deliberative thought processes that occur from initial recognition of a situation with ethical content to implementation of a justifiable action. The case scenario above provides an opportunity to explore a holistic framework, the Four Component Model (Rest, 1986), to identify and address ethical issues in nursing practice. The FCM describes the deliberative thought processes that occur from initial recognition of a situation with ethical content to implementation of a justifiable action: sensitivity, judgment, motivation, and action (Rest, 1986; Robichaux, 2012; Robichaux, 2017; Rushton & Penticuff, 2007).
Ethical Sensitivity
Ethical sensitivity is described as our ability to recognize an ethical problem, the moral implications of our decisions, and how our actions affect other people (Milliken, 2016). Its development depends on an understanding of the ethical nature of the role as an obligation of the nursing profession (Milliken & Grace, 2017). In the case scenario, Nancy recognized that adhering to the EHR-triggered CDS guideline might result in a poor outcome. She may have also been aware of her accountability in the situation as stated in the ANA Code of Ethics for Nurses with Interpretive Statements, “Systems and technologies that assist in clinical practice are adjunct to, not replacements for, the nurse’s knowledge and skill” (American Nurses Association [ANA], 2015, p.16; hereafter referred to as Code of Ethics). Having practiced in the ED for ten years, Nancy may be respected by her nursing peers and physician colleagues and may question how her actions could potentially affect those professional relationships.
Ethical Judgment
Not all issues will require an in-depth consideration of all elements in a specific model, and the goal is to reach a prudent choice, not certainty. The second component of the FCM is ethical judgment or decision-making, a deliberative process reflecting knowledge of ethical principles, theories, and codes. There are several models (see Table 2); most have elements that outline an approach to reaching a decision through identifying facts and considering specific questions related to ethical principles and/or virtue ethics and care ethics. Not all issues will require an in-depth consideration of all elements in a specific model, and the goal is to reach a prudent choice, not certainty (Grace, 2014; Milliken & Grace, 2017; Robichaux, 2017). Recognizing the potential harm of following the sepsis guidelines in a patient with suspected pulmonary edema, Nancy decides to share her concerns with the physician.
Table 2. Ethical Judgment/Decision-making Models
Internet Sources for Ethical Judgment/Decision-Making Models
The University of Washington School of Medicine. (2014). A case-based approach to ethical decision-making. Retrieved from https://depts.washington.edu/bioethx/tools/4boxes.html
Santa Clara University Markula Center for Applied Ethics. (2017). Ethical decision making. Retrieved from https://www.scu.edu/ethics/ethics-resources/ethical-decision-making/
Ethical Motivation
All nurses want to be ethical and live in a manner consistent with their personal and professional values. Although they may recognize an ethical issue and be aware of their role-associated obligations, personal and/or institutional barriers may impede their motivation to act. The third component in the FCM, ethical motivation is the bridge between decision-making and action (Robichaux, 2017).
Competing personal values. can impede motivation and action. Competing personal values such as protecting one’s position or reputation can impede motivation and action. “Persevering to do the right thing” (Grace, Robinson, Jurchak, Zollfrank, & Lee, 2014, p. 14) can also be hampered by institutional barriers. Lack of supervisory support, fear of reprisal, and hierarchal decision-making may silence nurses’ moral voices (Pavlish, Hellyer, Brown-Saltzman, Miers, & Squire, 2013). These obstacles may characterize a unit ethical climate that does not promote patient/family advocacy and nurse moral agency. Wolf et al. (2016) described the moral distress of ED nurses who are unable to meet their role obligations to provide safe and effective patient care in such environments.
The stress felt by Nancy in the presented ED case scenario is an example of this type of moral distress. Specific themes reflected in the case scenario and noted by Wolf and colleagues’ (2016) qualitative investigation relate to moral distress due to overemphasis on documentation, tasks, and metrics at the expense of patient care, as well as role conflicts resulting from hierarchical decision making. These same issues are reflected in a number of comments in Table 1 (e.g., overemphasis on documentation and measurement creating inefficiencies and a distraction to patient care).
Ethical Action
Nancy questions the physician’s decision to follow the sepsis quality metric and not write an order in the EHR for slow intravenous fluid administration. She verbally reports this information to the receiving ICU nurse and hopes “for the best outcome” for the patient. Could additional actions have been taken? Developing moral courage may assist in overcoming personal and institutional barriers to further nurse advocacy. Individuals with moral courage have developed skills of effective engagement and “willingness to speak out and do what is right in the face of forces that would lead a person to act in some other way” (Lachman, 2007, p. 131). Moral courage can also be “learned, practiced, and mentored” (Hawkins & Morse, 2014, p. 268). When moral courage and ethical action are thwarted by constraints outside the nurse's control, moral distress can result.
Nurses experience moral distress, a concept first highlighted by Andrew Jameton in 1984, when they "know the right thing to do while being in a situation in which it is nearly impossible to do it." (Jameton, 2017, p. 617). Jameton described three components that can apply to the pain expressed by the nurses that contributed to the Texas study: knowing what is right, being in a situation that constrains acting on that knowledge, and the psychological distress resulting from that inability to do the right thing (Jameton, 2017).
It may be challenging to remember what actions to take when encountering a situation that requires moral courage. It may be challenging to remember what actions to take when encountering a situation that requires moral courage (Lachman, 2010; Lachman, Murray, Iseminger, & Ganske, 2012) Lachman et al. (2012) have developed a useful mnemonic, CODE (Courage; Obligations to honor; Danger management; Expression), that reminds nurses of their ethical obligations and actions as detailed in the nursing Code of Ethics (ANA, 2015). The CODE mnemonic strategy helps nurses to recall these actions and includes ways to overcome fear and reluctance to speak up including reflection, reframing, and assertiveness skills.
The accelerated growth and adoption of the EHR has produced a situation that repeatedly occurs in the history of technology and parallels the rise of bioethics. The Code of Ethics states, “Patients’ rights are the primary factor in any decisions regarding personal information, whether from or about the patient. These rights of privacy and confidentiality pertain to all information in any manner that is communicated or transmitted” (ANA, 2015, p. 10). While nurses are aware of this ethical obligation in relation to the EHR, they may be less familiar with additional ethical issues inherent in its use and development. The accelerated growth and adoption of the EHR has produced a situation that repeatedly occurs in the history of technology and parallels the rise of bioethics. From cardiopulmonary resuscitation (CPR) to genetic engineering, the creation and use of an innovative tool may surpass the knowledge and resources required to ensure an ethical and appropriate use (Goodman, 2015).
The current and potential positive impact of the EHR on quality care is not disputed. However, ethical issues surrounding dominance of institutional priorities over autonomous patient-centered practice and care driven by application of decision-support, templates, and/or clinical practice guidelines (CPGs) have been documented (Lown & Rodriguez, 2012; McBride, Tietze, Hanley, & Thomas, 2015; Sulmasy, López, & Horwitch, 2017). Perhaps the most troubling ethical issue noted is the potential erosion of the patient-nurse relationship (de Ruiter, Liaschenko, & Angus, 2016; Rathert, Mittler, Banerjee, & McDaniel, 2016).
The centrality of the patient-nurse relationship to the nursing discipline is reflected in the interpretive statement, “The nurse’s primary commitment is to the recipients of nursing and health care services” (ANA, 2015, p. 5). Effective communication is vital to this relationship, and the EHR may have a negative effect. Research suggests that it can become a “third party “in the process, potentially reshaping the interaction, changing the patient narrative, and diverting nurse attention away from the patient (Rathert et al., 2016).
Perhaps the most troubling ethical issue noted is the potential erosion of the patient-nurse relationship. The use of computers and communication technologies will impact more lives in the 21st century than any other technology, including stem cells, transplants, and nanomedicine (Goodman, 2015). As the largest group of healthcare professionals who document, more than any other discipline in acute care organizations, (OʼBrien, Weaver, Settergren, Hook, & Ivory, 2015) nurses are at the forefront to ensure that the EHR is patient-centered and contributes to safe, ethical practice.
As indicated in the case scenario and the study findings, the use of the EHR can result in a unique set of ethical and legal challenges. Nurses must be prepared to face these challenges and recognize the requirements of state and federal law, workplace policies, and obligations of the profession. A study in 2006 revealed that nurses spent a majority of indirect nursing time documenting in the EHR, demonstrating the critical necessity of proper usage to satisfy quality of patient care (Kim, 2006). The Scope and Standards of Nursing Practice (ANA, 2015) establishes the standard of practice for registered nurses in the United States, noting “Nurses must document relevant data accurately and in a manner accessible to the interprofessional team” (ANA, 2015, p. 54). Documentation in the nursing record must follow principles of “factuality, accuracy, completeness, timeliness, organization, and compliance” (ANA, 2015, p. 270). Documentation must be clear and accurate to provide a basis for the contribution of nurses to patient outcomes and the viability of healthcare organizations (ANA, 2015).
Documentation that fails to meet these principles can result in undesirable outcomes for the nurse, patients and families, or for the healthcare organization (ANA, 2015). Nursing documentation, electronic or handwritten, are legal documents that can, under some circumstances, be used in legal proceedings. Nurses maintain competence regarding the legal significance of documentation and therefore must demonstrate legible and comprehensive reporting (Larsen, 2012). Some EHR systems are designed as templates or ‘fill-in’ instruments, which allow for auto-population of lab results or other critical information (Sittig & Singh, 2011). The auto-fill function can result in unintentional documentation of a clinical finding that may not be within a nurse's clinical purview (Sittig & Singh, 2011). Once documentation has been electronically recorded and signed by the nurse, the liability of that acknowledgement is not clear.
A number of healthcare organizations have implemented ‘copy and paste’ policies for documenting in the EHR. The copy and paste functionality includes copying, pasting, cloning, auto-filling, carrying forward, replicating data and reusing content from one section to another within the EHR (Scruth, 2014). The copy and paste phenomenon has caused significant debate from those who argue its necessity for time efficiency weighed against the significant risk of inaccuracy and patient safety errors (Harrington, 2017). Copy and paste functionalities can result in unintentional reliance on outdated or inaccurate clinically relevant information, such as treatment plan; distracted notes; diagnostic biases; incorrect information for a specific patient visit; and expired patient symptoms and assessments (Scruth, 2014; Weis & Levy, 2014). These practices can result in timeliness issues or time-related accuracy of documentation in any EHR.
. healthcare providers have experienced notable challenges to balance necessary time for patient care with computer entry. EHRs are designed to facilitate easier provider order entry and have been shown to reduce prescription errors (Scruth, 2014). They have tremendous potential to improve efficiency of healthcare delivery and improvement of quality patient care. However, healthcare providers have experienced notable challenges to balance necessary time for patient care with computer entry (McBride et al., 2017; Wolf et al., 2016). In the early 1990s ‘charting by exception’ was an acceptable method to decrease charting in nursing (de Ruiter et al., 2016). Historically, it was assumed that all standards of care were met unless documented otherwise. However, with the introduction of the EHR, complete documentation requires charting of all clinical assessments, care plans, interventions, and outcomes requiring more time for documentation (de Ruiter et al., 2016).
As a result of time constraints and usability issues, nurses have reportedly been intentionally entering false information to bypass or ‘work-around’ EHR systems (McBride & Tietze, 2017). Although privacy, security, and confidentiality have been identified as three main areas of concern when using EHRs, little attention has focused on false entries, work-arounds, or system bypasses (Ayatollahi, Mirani, & Haghani, 2014; CMPA, 2015).
. a false entry into an EHR can follow a patient for years. Additionally, alert fatigue and clinical information overrides must be addressed within the organization. Legal concerns over notification of federally regulated drug interactions, through pop-ups or alerts, can be overwhelming or desensitizing to the nurse (Sittig & Singh, 2011). Overriding content in what is often an undesirable system design can result in misinformation in charting that can have detrimental effects on the nurse, patient, and healthcare organization. For example, a false entry into an EHR can follow a patient for years. The patient is likely unaware of the false entry, but subsequently applies for health or life insurance. The patient may be denied insurance coverage based on a one-time false entry that was replicated over time.
We conclude with a call to action for interprofessional teams, associations, industry, and others to collaboratively address these issues on behalf of the health and safety of the nation, and equally as important, the health and well-being of the healthcare workforce. To do that, the authors suggest the following recommendations to address challenges with EHRs. These recommendations may help mitigate ethical and legal issues arising as a result of the massive uptake of technology that has resulted in the digital age of healthcare delivery.
Support
Nurses must have a seamless mechanism for reporting EHR challenges. Nurses face time constraints, overstaffing, and unfamiliarity with EHR systems on a daily basis. Healthcare organizations must have structures in place at the unit, management, and administrative levels to facilitate effective use of EHRs in nursing practice. For example, some EHR contracts have “hold harmless clauses” which restrict nurses’ ability to effectively and timely report EHR problems (Sittig & Singh, 2011). Nurses must have a seamless mechanism for reporting EHR challenges (e.g., inappropriate or cumbersome alerts) without an arduous process or fear of reprisal. This type of support could potentially mitigate the moral distress noted in the case scenario.
Culture of Safety
Nurse managers and executives have a particular obligation to ensure that direct care nurses are empowered to identify and engage in ethical situations associated with EHRs. All nurses are “responsible for contributing to a moral environment” in healthcare (ANA, 2015, p. 24). Nurse managers and executives have a particular obligation to ensure that direct care nurses are empowered to identify and engage in ethical situations associated with EHRs. The ANA Scope and Standards of Practice for Nursing Administration (2009) cites the obligation of nurse administrators to advocate for practice that reflects the Code of Ethics (ANA, 2015). It specifies duties that nurses in leadership and managerial roles have, particularly in transformational and servant leadership frameworks, to open communication and to act “entirely on the behalf of those led” (ANA, 2009, p. 8) to identify problems and integrate ethical provisions in all areas of practice. Nurses in administrative roles should promote a culture of safety in their settings that include reducing the risk of harm arising from inadequate EHR design, and usability (ANA, 2009).
Education
Studies have shown that nurses with one year or less in practice demonstrate almost 70% more timely charting than nurses with more years of experience (Ahn, Choi, & Kim, 2016). This emphasizes the need for continuing education for novice and expert nurses in EHR management and documentation. Informatics specialty nurses and advanced practice nurses can serve as leaders to assess and research documentation for timeliness and accuracy, along with providing continuing education on a frequent basis (Scruth, 2014). Education about principles of documentation and competence in specific EHR system usage is needed to foster nurse mastery and development to successfully improve health outcomes (Goodman, 2015).
Awareness of Support of Interprofessional Imperatives
Guidelines and best practices, such as the American College of Physicians position paper on clinical documentation (Kuhn, Basch, Barr, & Yackel, 2015), ANA (2015) position statement on Privacy and Confidentiality,and American Nursing Informatics Association (2015) position statement on Addressing the Safety of Electronic Health Records are critical to ensuring that nurses are able to efficiently and appropriately meet principles of documentation. The American Health Information Management Association (AHIMA, 2011) Code of Ethics has 11 principles with interpretive statements, referred to as guidelines, that seem to underscore the importance of practices that stand in stark contrast to the experiences of nurse participants in the Texas nursing research (McBride et al., 2015). The AHIMA principles cite the primacy of accuracy, avoidance of conflicts of interest, and similar to the ANA code, “respect [for] the inherent dignity and worth of every person” (AHIMA, 2011, 11). Under this AHIMA principle, the noteworthy guideline to “ensure all voices are listened to and respected” (AHIMA, 2011, 11.4) demands that health information managers not only welcome input from nurses who find the technological determinism of EHRs violates ethical practice and clinical judgment, but also seek out that input.
. the patient’s story of his/her illness may be lost to the goal of generating standard data points that, in turn, trigger algorithms and practice recommendations. For care characterized by “screen-driven information gathering” (Lown & Rodriguez, 2012, p. 393) the patient’s story of his/her illness may be lost to the goal of generating standard data points that, in turn, trigger algorithms and practice recommendations (Brown, 2015). This computational capacity may establish EHR information as authoritative, potentially displacing work processes critical to nurse-patient interaction.
As evidenced in the study themes and the case scenario presented, critical thinking may be hindered and experiential knowledge devalued (Campbell & Rankin, 2017). Most importantly, the EHR must not substitute for a current and accurate clinical assessment, and appropriate intervention (Campbell & Rankin, 2017; Lown & Rodriguez, 2012; Sulmasy et al., 2017). Systems and technologies such as EHRs that assist in clinical practice are adjunct to, not replacements for, nurse knowledge and skill (ANA, 2015).
Most importantly, the EHR must not substitute for a current and accurate clinical assessment, and appropriate intervention. Finally, as reflected in the Texas study and clinical scenario, current technology in the healthcare industry often presents challenges with usability, design, implementation, and failure to adequately support clinical teams. This results in ethical situations often associated with feelings of moral distress. Application of the FCM can assist clinical teams to explore and potentially resolve these issues. Additionally, the authors recommend further research into the moral distress noted in emerging evidence, including the TNA-TONE statewide study and the case scenario presented. As such, the healthcare industry has an imperative to identify and address ethical issues with use of EHRs.
The authors wish to acknowledge the support for the study by Texas Nurses Association (TNA) and the Texas Organization of Nurse Executive (TONE). From the beginning in 2010 when the TNA Board of Directors resolution was passed, the two organizations created the partnership that provided cumulative guidance, funding, and dissemination efforts throughout the years. Specifically, we would like to acknowledge the staff of these organizations, the dozens of volunteer committee members who have served, and the report writing sub-committee of Susan McBride, Mary Anne Hanley, Cindy Zolnierek, Laura Thomas, Mari Tietze, and Huaxin Song. Finally, we acknowledge the many subject-matter experts who, through numerous focus groups, helped yield the final surveys. Please see the TNA/TONE HIT Web site for the long list of names.
Susan McBride, PhD, RN-C, CPHIMS, FAAN
Email: susan.mcbride@ttuhsc.edu
Dr. McBride is a Professor at the Texas Tech University Health Sciences Center School of Nursing whose research focus is on methods development for implementing, evaluating and utilizing health information technology to address patient safety, quality and population health. Dr. McBride was the Principal Investigator for a Texas Statewide Study of Nurses Satisfaction with their electronic health records. She is a professor with teaching responsibilities supporting graduate courses in statistics, informatics, and epidemiology. She is a Fellow in the Academy of Nursing and sits on the Information Technology and Informatics Expert Panel.
Mari Tietze, PhD, RN-BC, FHIMSS
Email: mtietze@twu.edu
Dr. Tietze is a Professor at the Texas Woman's University (TWU) College of Nursing, teaching informatics courses focused on interprofessional collaborative practice and Director of the Graduate Certificate in Interprofessional Informatics program. Dr. Tietze is the Doswell Endowed Chair for Nursing Informatics aimed at advancing nursing informatics at TWU. Since 2010, she has been the co-chair of the Texas Nurses Association/Texas Organization of Nurse Executives Health Information Technology committee to represent nurses' experiences related to information technology use in their practice of patient care delivery. Research focus is telehealth with a telemedicine, remote management and mobile health component. Dr. Tietze has been certified since 2000 by ANA in Informatics Nursing.
Catherine Robichaux, PhD, RN, APRN, Alumna CCRN
Email: robichaux@uthscsa.edu
Dr. Robichaux is an Adjunct Assistant Professor at University of Texas Health; San Antonio, Texas and The University of Mary in Bismarck, North Dakota. She has taught ethics at the undergraduate and graduate levels and conducted research on moral distress and ethical climate among other issues. Catherine was a member of the Steering Committee to revise the Code of Ethics and is currently a member of the ANA Ethics Advisory Board.
Liz Stokes, JD, MA, RN
Email: liz.stokes@ana.org
Ms. Stokes is the Director of the American Nurses Association Center for Ethics and Human Rights. She worked for several years as a critical care nurse and later received her law degree. She worked as a consultant for the D.C. Board of Nursing interpreting professional ethics provisions and recently completed her masters in bioethics. Her leadership is demonstrated through various charitable roles. Liz serves as an Associate Editor for the Journal of Bioethical Inquiry and is a volunteer with the D.C. Bar Association. She is currently an American Academy of Nursing Jonas Health Policy Scholar.
Eileen Weber, DNP, JD, BSN, PHN, RN
Email: weber058@umn.edu
Dr. Weber is a nurse attorney and Clinical Assistant Professor at the University of Minnesota School of Nursing, where she teaches ethics, leadership, and public policy in the context of a continuum of interprofessional healthcare. She founded and leads the Upper Midwest Healthcare Legal Partnership Learning Collaborative. She serves on the American Nurses Association Center for Ethics and Human Rights Advisory Board and the University of Minnesota Medical Center (Fairview) ethics committee.
Office of National Coordinator for Health Information Technology. (2017). Health IT dashboard:
Quick stats. Retrieved from https://dashboard.healthit.gov/quickstats/quickstats.php
Ahn, M., Choi, M., & Kim, Y. (2016). Factors associated with the timeliness of electronic nursing documentation. Healthcare Informatics Research, 22(4), 270. doi:10.4258/hir.2016.22.4.270
American Health Information Management Association (AHIMA). (2011). AHIMA Code of Ethics. Retrieved from http://bok.ahima.org/doc?oid=105098#.WmtkOmQ-doE
American Nurses Association. (2009). Nursing administration: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association. Retrieved from http://www.r2library.com/resource/title/9781558102675
American Nurses Association. (2015). Code of ethics for nurses with interpretive statements (2nd ed.). Silver Spring, MD: American Nurses Association. Retrieved from http://www.r2library.com/resource/title/9781558105997
American Nursing Informatics Association. (2015). Addressing the safety of electronic health records: Position statement. Retrieved from https://www.ania.org/about-us/position-statements/addressing-safety-electronic-health-records
Ayatollahi, H., Mirani, N., & Haghani, H. (2014). Electronic health records: What are the most important barriers? Perspectives in Health Information Management / AHIMA, American Health Information Management Association, 11, 1c. Retrieved from http://perspectives.ahima.org/electronic-health-records-what-are-the-most-important-barriers/
Brown, D. L. (2015). Rethinking the role of clinical practice guidelines in pharmacy education. American Journal of Pharmaceutical Education, 79(10), 148. doi:10.5688/ajpe7910148
Campbell, M. L., & Rankin, J. M. (2017). Nurses and electronic health records in a Canadian hospital: Examining the social organisation and programmed use of digitised nursing knowledge. Sociology of Health & Illness, 39(3), 365-379. doi:10.1111/1467-9566.12489
De Ruiter, H., Liaschenko, J., & Angus, J. (2016). Problems with the electronic health record. Nursing Philosophy, 17(1), 49-58. doi:10.1111/nup.12112
Goodman, K. W. (2015). Ethics, medicine, and information technology: Intelligent machines and the transformation of health care (2nd ed.). Cambridge, England: Cambridge University Press.
Grace, P. (2014). Nursing ethics and professional responsibility in advanced practice (2nd ed.). Burlington, MA: Jones & Bartlett Learning.
Grace, P., Robinson, E., Jurchak, M., Zollfrank, A., & Lee, S. (2014). Clinical ethics residency for nurses: An education model to decrease moral distress and strengthen nurse retention in acute care. JONA: The Journal of Nursing Administration, 44(12), 640-646. doi:10.1097/NNA.0000000000000141
Harrington, L. (2017). Copy-forward in electronic health records: Lipstick on a pig. The Joint Commission Journal on Quality and Patient Safety, 43(8), 371-374. Retrieved from doi:10.1016/j.jcjq.2017.04.007
Hawkins, S. F., & Morse, J. (2014). The praxis of courage as a foundation for care. Journal of Nursing Scholarship, 46(4), 263-270. doi:10.1111/jnu.12077
Healthy Aging Team. (2017). 10 most chronic conditions in adults 65+. Retrieved from https://www.ncoa.org/resources/10-common-chronic-conditions-adults-65/
Henry, J., Pylypchuk, Y., Searcy, T., & Patel, V. (2016). Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008-2015. Washington, DC: Office of National Coordinator for Health IT. Retrieved from https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php
Jameton, A. (2017). What moral distress in nursing history could suggest about the future of health care. AMA Journal of Ethics 19(6), 617-628. doi:10.1001/journalofethics.2017.19.06.mhst1-1706.
Kim, D. Y. (2006). Analysis of nurse's job in general hospital using hospital information system after introduction of electronic nursing record system. Available from Keimyung University, Deagu, Korea. (Master's Thesis).
Kuhn, T., Basch, P., Barr, M., & Yackel, T. (2015). Clinical documentation in the 21st century: Executive summary of a policy position paper from the American college of physicians. Annals of Internal Medicine, 162(4), 301. doi:10.7326/M14-2128
Lachman, V. D. (2010). Strategies necessary for moral courage. Online Journal of Issues in Nursing, 15(3), Manuscript 3. doi:10.3912/OJIN.Vol15No03Man03
Lachman, V. D. (2007). Moral courage in action: Case studies. Medsurg Nursing: Official Journal of the Academy of Medical-Surgical Nurses, 16(4), 275. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17907703
Lachman, V. D., Murray, J. S., Iseminger, K., & Ganske, K. M. (2012). Doing the right thing: Pathways to moral courage. American Nurse Today, 7(5), 1-6. Retrieved from https://www.americannursetoday.com/doing-the-right-thing-pathways-to-moral-courage/
Larsen, A. (2012). Trappings of technology: Casting palliative care nursing as legal relations. Nursing Inquiry, 19(4), 334-344. doi:10.1111/j.1440-1800.2011.00568.x
Lown, B. A., & Rodriguez, D. (2012). Commentary: Lost in translation? How electronic health records structure communication, relationships, and meaning. Academic Medicine: Journal of the Association of American Medical Colleges, 87(4), 392. doi:10.1097/ACM.0b013e318248e5ae
McBride, S., Tietze, M., Hanley, M. A., & Thomas, L. (2015). Statewide study assessing the experience of nurses with their electronic health records. Austin, TX: Texas Nurses Association. Retrieved from https://c.ymcdn.com/sites/www.texasnurses.org/resource/resmgr/HIT_Files/HIT_Survey_Report-Final.pdf
McBride, S., Tietze, M., Hanley, M. A., & Thomas, L. (2017). Statewide study to assess nurses' experiences with meaningful use-based electronic health records. CIN: Computers, Informatics, Nursing, 35(1), 18-28. doi:10.1097/CIN.0000000000000290
McBride, S., Zolnierek, C., Tietze, M. F., Hanley, M. A., Thomas, L., & Song, H. (2015). Statewide study assessing the experience of nurses with their electronic health records. (No. TNA/TONE2015). Austin, TX: Texas Nurses Association. Retrieved from http://www.texasnurses.org/?page=HIT
Milliken, A. (2016). Nurse ethical sensitivity: An integrative review. Nursing Ethics, 2016(May), 1-3. doi:10.1177/0969733016646155
Milliken, A., & Grace, P. (2017). Nurse ethical awareness: Understanding the nature of everyday practice.Nursing Ethics, 24(5), 517-524. doi:10.1177/0969733015615172
Office of National Coordinator for Health Information Technology. (2017). Health IT dashboard:
Quick stats. Retrieved from https://dashboard.healthit.gov/quickstats/quickstats.php
OʼBrien, A., Weaver, C., Settergren, T. T., Hook, M. L., & Ivory, C. H. (2015). EHR documentation: The hype and the hope for improving nursing satisfaction and quality outcomes. Nursing Administration Quarterly, 39(4), 333-339. doi: 10.1097/NAQ.0000000000000132
Osheroff, J. A., Teich, J. M., Levick, D., Saldana, L., Velasco, F. T., Sittig, D. F., . . . Jenders, R. A. (2012). Improving outcomes with CDS: An implementer’s guide (2nd ed.). Chicago, IL: Healthcare Information and Management Systems Society. Retrieved from http://www.himss.org/ResourceLibrary/ResourceDetail.aspx?ItemNumber=11590
Pavlish, C., Hellyer, J., Brown-Saltzman, K., Miers, A., & Squire, K. (2013). Barriers to innovation: Nursesʼ risk appraisal in using a new ethics screening and early intervention tool. Advances in Nursing Science, 36(4), 304-319. doi:10.1097/ANS.0000000000000004
Rathert, C., Mittler, J. N., Banerjee, S., & McDaniel, J. (2016). Patient-centered communication in the era of electronic health records: What does the evidence say? Patient Education and Counseling, 100(1), 50-64. doi:10.1016/j.pec.2016.07.031
Rest, J. R. (1986). Moral development: Advances in research and theory. New York: Praiger. Retrieved from http://catalog.hathitrust.org/Record/000441705
Robichaux, C. (2012). Developing ethical skills: From sensitivity to action. Critical Care Nurse, 32(2), 65-72. doi:10.4037/ccn2012929
Robichaux, C. (2017). Ethical competence in nursing practice: Competencies, skills, decision-making (1st ed.). New York: Springer Publishing Company.
Rushton, C. H., & Penticuff, J. H. (2007). A framework for analysis of ethical dilemmas in critical care nursing.AACN Advanced Critical Care, 18(3), 323-328. doi:10.1097/01.AACN.0000284434.83652.d5
Scruth, E. (2014). Quality nursing documentation in the medical record. Clinical Nurse Specialist, 28(6), 312-314. doi:10.1097/NUR.0000000000000085
Sittig, D. F., & Singh, H. (2011). Legal, ethical, and financial dilemmas in electronic health record adoption and use. Pediatrics, 127(4), e1047. doi:10.1542/peds.2010-2184
Sulmasy, L., López, A., & Horwitch, C. (2017). Ethical implications of the electronic health record: In the service of the patient. Journal of General Internal Medicine, 32(8), 935-939. doi:10.1007/s11606-017-4030-1
U.S. Department of Health and Human Services. (2012). HITECH act enforcement interim final rule. Retrieved from http://www.hhs.gov/hipaa/for-professionals/special-topics/HITECH-act-enforcement-interim-final-rule/
Weis, J. M., & Levy, P. C. (2014). Copy, paste, and cloned notes in electronic health records: Prevalence, benefits, risks, and best practice recommendations. Chest, 145(3), 632. doi:10.1378/chest.13-0886
Wolf, L. A., Perhats, C., Delao, A. M., Moon, M. D., Clark, P. R., & Zavotsky, K. E. (2016). "It's a burden you carry": Describing moral distress in emergency nursing. Journal of Emergency Nursing: JEN: Official Publication of the Emergency Department Nurses Association, 42(1), 37. doi: 10.1016/j.jen.2015.08.008
Figure 1. Major and minor themes related to qualitative study comments.
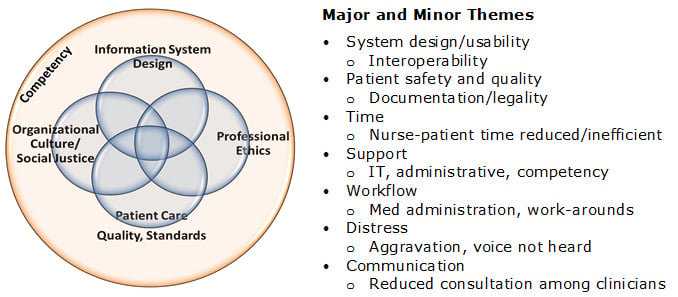
Table 1. Comments by Nurses about their EHR Experience
Category
Comment
Training
I have almost no training on the "System.” I have to fumble around to do anything on this "System" and it is purely an accident when I do find what I need.
Documentation
System was not designed by the people who would use it. It does not capture the data required by the state to successfully use it. We are unable to see any notes/assessments that we did not personally input. Very frustrating because we constantly have to do double work.
Sometimes the canned responses to questions do not have the appropriate answer listed as an option, and the only way to complete the documentation is to go to another menu and enter a nurse’s note. Our preop department uses entries in both the nursing module and the OR module, which necessitates constantly switching from one menu to another - time consuming and inefficient.
The "copy/paste" function has made it easier for providers to not write new original assessments. Because most of the notes are copy and pasted, there are many discrepancies (on one line, the patient is intubated; on the next line of the same patient, the patient is on nasal cannula). It's made the notes semi-worthless.
This system has quadrupled our workload. It is not accurate and orders tend to disappear. The pharmacy part allows expired orders to carry on and continue to be active even after stop dates which lead to medication errors. This system is difficult to view orders and communicate with others. Things do not work well. It takes several hours to get thru discharges due to links that do not work. With the ER after two weeks on the program, it developed an application error that would not let nurses go back to add information while the patient is still active and document is active.
Equipment
Our computers at times freeze inside the room. During am med pass, it is so stressful finding a good computer that does not freeze. Sometimes I have to go through 3-5 computers before finding one that works.
Critical Thinking
Sometimes I feel that the barcode scanning system for medication administration hinders critical thinking and prevents truly looking at what you are giving the patient.
Table 2. Ethical Judgment/Decision-making Models
Internet Sources for Ethical Judgment/Decision-Making Models
The University of Washington School of Medicine. (2014). A case-based approach to ethical decision-making. Retrieved from https://depts.washington.edu/bioethx/tools/4boxes.html
Santa Clara University Markula Center for Applied Ethics. (2017). Ethical decision making. Retrieved from https://www.scu.edu/ethics/ethics-resources/ethical-decision-making/
January 31, 2018
DOI: 10.3912/OJIN.Vol23No01Man05